If you or your child are battling persistent nasal congestion, a constantly runny nose, or unexplained ear infections, you might be dealing with a common but often overlooked condition: adenoiditis. Inflammation of the adenoids can be the hidden culprit behind a frustrating array of symptoms. This comprehensive guide will walk you through everything you need to know about adenoiditis—its causes, symptoms, diagnosis, and treatment options—to help you breathe easier and find lasting relief.
What Are Adenoids, and What is Adenoiditis?
First, let’s clarify a common point of confusion. The keyword “adenoidid” likely refers to adenoiditis—the medical term for inflamed or infected adenoids.
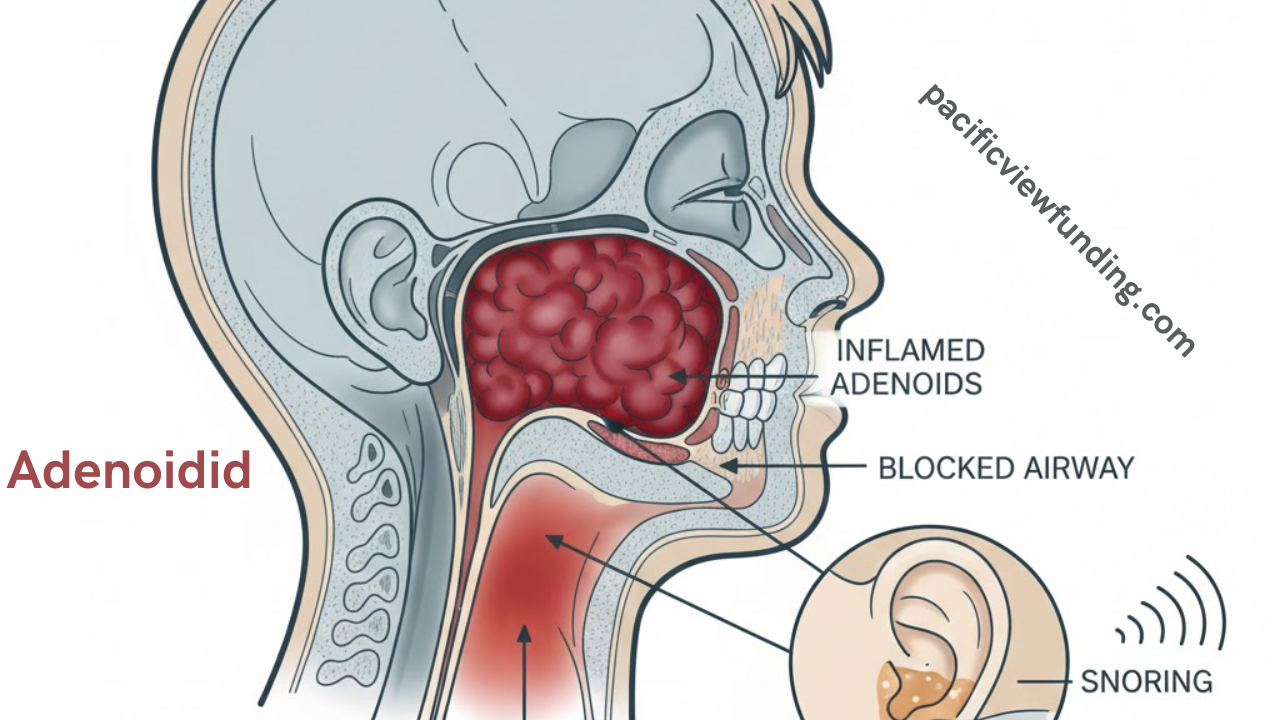
The adenoids are a small patch of tissue made of lymphoid cells, similar to tonsils, located high in the throat behind the nose and the roof of the mouth (nasopharynx). They are part of the immune system’s first line of defense, helping to trap germs entering through the nose and mouth, especially in young children.
Adenoiditis occurs when this tissue becomes swollen and inflamed due to infection, allergies, or other irritants. While adenoids are beneficial in early childhood, they often shrink and become less active after age 5, typically disappearing by the teenage years. However, when they become chronically infected or overly enlarged, they can cause significant health issues.
Symptoms: How to Recognize Adenoiditis
The symptoms of inflamed adenoids can be varied and sometimes mistaken for other conditions like the common cold, sinusitis, or allergies. They are generally categorized by how they affect different connected systems.
Nasal and Breathing Symptoms
-
Chronic Nasal Congestion: A persistent stuffy nose, leading to mouth breathing.
-
Runny Nose: Persistent post-nasal drip or a runny nose with clear or greenish discharge.
-
Snoring and Loud Breathing: Significant, loud snoring is a hallmark of enlarged adenoids.
-
Sleep Apnea: Pauses in breathing during sleep, often leading to restless sleep, night sweats, and bedwetting in children.
-
Altered Speech: A nasal, “blocked” sound to the voice, as if the person is always speaking with a cold.
Ear-Related Symptoms
-
Recurrent Ear Infections: The swelling can block the Eustachian tubes, which connect the middle ear to the throat, leading to fluid buildup and infections (otitis media).
-
Glue Ear: Persistent fluid in the middle ear without infection, which can cause temporary hearing loss.
-
Ear Pain: A frequent complaint due to pressure imbalance and infection.
Throat and General Symptoms
-
Sore Throat: Difficulty swallowing and a persistent raw feeling in the throat.
-
Swollen Neck Glands: Tender lymph nodes in the neck.
-
“Adenoid Facies”: A long-term open-mouth posture can affect facial development in children, leading to a characteristic elongated face and dental issues.
-
Poor Sleep Quality: Leading to daytime fatigue, irritability, and learning or behavioral problems in kids.
Primary Causes and Risk Factors of Adenoid Inflammation
Understanding what triggers adenoiditis is key to prevention and treatment.
-
Infections: The most common cause. Viral infections (like the common cold, flu, or Epstein-Barr) or bacterial infections (commonly Streptococcus) can lead to acute or chronic inflammation.
-
Allergies: Chronic exposure to allergens like pollen, dust mites, or pet dander can cause the adenoid tissue to remain permanently swollen.
-
Chronic Sinusitis: A continuous cycle of sinus infection and inflammation can spread to the adenoid tissue.
-
Gastroesophageal Reflux Disease (GERD): Stomach acid irritating the back of the throat can lead to adenoid swelling.
-
Age: Adenoid issues are most prevalent in children aged 3-7, when the tissue is at its largest and most active.
-
Environmental Irritants: Smoke, pollution, and chemical fumes can contribute to chronic irritation.
Diagnosis: How Doctors Identify Adenoiditis
If you suspect adenoid problems, a visit to an ENT (Ear, Nose, and Throat) specialist is crucial. Diagnosis typically involves:
-
Medical History and Symptom Review: The doctor will ask detailed questions about sleep, breathing, and infection history.
-
Physical Examination: While adenoids can’t be seen by looking in the mouth, the doctor will examine the throat, ears, and neck lymph nodes.
-
Nasal Endoscopy: A key diagnostic tool. A thin, flexible tube with a light and camera is gently passed through the nose to visualize the size and condition of the adenoid tissue directly.
-
X-ray or CT Scan: In some cases, imaging of the side of the neck can help assess the degree of enlargement and its impact on the airway.
-
Sleep Study (Polysomnography): For suspected sleep apnea, an overnight study monitors breathing, oxygen levels, and sleep cycles.
Treatment Options: From Home Care to Surgery
Treatment for adenoiditis depends on whether the condition is acute (short-term) or chronic, the severity of symptoms, and the patient’s age.
Conservative and Medical Management
For mild or acute cases, non-surgical approaches are always tried first:
-
Nasal Corticosteroid Sprays: Like fluticasone, to reduce inflammation and swelling directly.
-
Antibiotics: Prescribed for confirmed bacterial infections.
-
Antihistamines or Allergy Medications: To manage underlying allergic triggers.
-
Saline Nasal Rinses: Helps clear mucus and reduce post-nasal drip.
-
Humidifiers and Hydration: Moist air and plenty of fluids can soothe irritated tissues.
Surgical Intervention: Adenoidectomy
When medical management fails and symptoms are severe—such as in cases of obstructive sleep apnea, recurrent ear infections, or significant breathing difficulties—an adenoidectomy may be recommended.
This is a common, safe surgical procedure to remove the adenoids. It is often done alongside a tonsillectomy if the tonsils are also problematic.
-
The Procedure: Performed under general anesthesia, usually taking about 30 minutes. The surgeon removes the tissue through the mouth, leaving no external scars.
-
Recovery: Typically involves a 7-10 day recovery period with a soft-food diet, increased fluid intake, and management of temporary throat pain and bad breath.
-
Benefits: Provides immediate relief from nasal obstruction, often resolving chronic ear fluid, sinusitis, and sleep apnea. The immune system functions normally without the adenoids, as other lymphoid tissues take over.
Potential Complications of Untreated Adenoiditis
Ignoring chronic adenoid inflammation can lead to more serious issues:
-
Chronic Sinus and Ear Infections: Leading to potential hearing loss or speech delays.
-
Sleep-Disordered Breathing: Chronic sleep apnea can affect oxygen levels, leading to cardiovascular strain, poor growth, and cognitive/behavioral issues in children.
-
Facial Development Changes: The long-term mouth breathing associated with enlarged adenoids can alter jaw and palate development.
-
Poor Quality of Life: Persistent fatigue, missed school or work, and general discomfort.
When to Seek Medical Advice
Consult a healthcare professional if you or your child experience:
-
Breathing difficulties, especially pauses during sleep.
-
Symptoms lasting more than 10-14 days without improvement.
-
Recurrent ear or sinus infections (more than 3-4 per year).
-
Significant snoring accompanied by restless sleep.
-
Concerns about hearing or speech development.
Conclusion: Taking Control of Adenoid Health
Adenoiditis, while common, is a treatable condition. Whether it manifests as a simple recurrent sore throat or complex sleep apnea, understanding the signs and seeking appropriate evaluation is the first step toward resolution. From simple nasal sprays to the definitive solution of an adenoidectomy, modern medicine offers effective pathways to restore clear breathing, peaceful sleep, and overall well-being.
Don’t let unexplained symptoms become your new normal. Persistent nasal congestion, snoring, and ear troubles are your body’s signals that something needs attention.